In this article
Have you ever wondered what dry eyes and a dry mouth have in common with hypothyroidism? Surprisingly, more than you might think. These dryness-related symptoms are common symptoms of Sjogren’s syndrome, an autoimmune disorder. And research suggests there is a link between Sjogren’s syndrome and hypothyroidism.
While these two health conditions may seem quite different on the surface, they share an intriguing connection. Ahead, we’ll learn about this connection and why having one condition may increase the likelihood of developing the other.
Sjogren’s syndrome is a complex autoimmune disorder that targets the exocrine glands in your body. Exocrine glands produce and secrete secretions directly into an area of your body. For instance, salivary glands, a type of exocrine gland, secrete saliva into your mouth. Other examples of exocrine glands are lacrimal (tear ducts), sweat, and mammary glands.
When your immune system mistakenly attacks these glands, these glands can no longer function effectively. Sjogren’s syndrome primarily affects the salivary and tear glands, leading to dry mouth and eyes. However, for a subset of patients, Sjogren’s can also affect other parts of the body, including the joints, skin, and internal organs.
Symptoms of Sjogren’s syndrome
Symptoms of Sjogren’s syndrome include the following:
Dry eyes: One of the most common symptoms of Sjogren’s syndrome is dry eyes. This can cause a gritty or burning sensation, redness, and sensitivity to light. Your eyes might feel constantly irritated, which can lead to blurred vision over time.
Dry mouth: Sjogren’s syndrome can also cause dryness in the mouth, leading to difficulty swallowing or speaking. A persistent dry mouth can increase the risk of dental decay, cavities, and oral infections. You may experience a sticky or cotton-like feeling in your mouth and have difficulty tasting or chewing food. In some cases, laryngitis and trouble swallowing may also develop.
Fatigue: Chronic fatigue is frequent in individuals with Sjogren’s syndrome. This overwhelming tiredness can be debilitating and affect daily activities. It is often accompanied by joint pain, muscle weakness, and a general feeling of malaise.
Joint pain and swelling: Joint pain and inflammation are common symptoms of Sjogren’s syndrome. This condition can affect multiple joints, leading to stiffness, swelling, and discomfort. The pain can range from mild to severe and may worsen with movement or overuse.
Skin and vaginal dryness: Apart from eyes and mouth, Sjogren’s syndrome can also cause dryness in other areas of the body, including the skin and vagina. Dry, itchy skin and recurrent vaginal infections are common symptoms that should not be ignored.
Digestive problems: Some individuals with Sjogren’s syndrome may experience digestive issues such as acid reflux, abdominal pain, and difficulty swallowing. These symptoms can significantly impact the quality of life and require medical attention.
Systemic symptoms: In some cases, Sjogren’s syndrome can affect organs other than the eyes and mouth. Individuals might experience symptoms such as recurrent sinus infections, lung problems, kidney dysfunction, and even neurological issues like peripheral neuropathy.
Here’s what you need to know about how Sjogren’s syndrome is diagnosed.
Consultation with a healthcare professional
The first step in diagnosing Sjogren’s syndrome is to schedule an appointment with a healthcare professional, preferably a rheumatologist, with specialized knowledge and experience in diagnosing autoimmune disorders. The healthcare professional will discuss your symptoms and medical history during this consultation and perform a physical examination.
Medical history and symptom analysis
The healthcare professional will ask comprehensive questions about your symptoms, including the frequency, duration, and intensity. They will also inquire about any other medical conditions you may have, as autoimmune disorders often present with overlapping symptoms. Providing accurate and detailed information will help the healthcare professional make an accurate diagnosis.
Blood tests
Blood tests are a crucial part of the diagnostic criteria for Sjogren’s syndrome. These tests measure the levels of specific antibodies and other markers in your blood that are associated with the disorder. The two primary antibodies tested for are anti-Ro/SSA and anti-La/SSB antibodies. The presence of these antibodies can confirm the presence of Sjogren’s syndrome.
Immunological tests
To further support the diagnosis, immunological tests may be conducted. These tests evaluate the functioning of the immune system and help identify any abnormalities or dysfunctions. Examples of immunological tests include checking the levels of immunoglobulins, complement proteins, and the erythrocyte sedimentation rate (ESR).
Eye and mouth evaluation
Since dry eyes and dry mouth are hallmark symptoms of Sjogren’s syndrome, a comprehensive exam of these areas may be conducted. This exam may involve eye exams to determine tear production, including the Schirmer’s test, and oral exams to assess saliva production.
Biopsy
In some cases, a minor salivary gland biopsy may be recommended to confirm the diagnosis of Sjogren’s syndrome. This involves removing a small piece of tissue from the lip or inside the cheek and examining it under a microscope for characteristic abnormalities.
It is important to note that the diagnosis of Sjogren’s syndrome can sometimes be challenging, as symptoms vary from person to person and can overlap with other conditions. Therefore, consulting with a healthcare professional with expertise in autoimmune disorders is crucial to ensure an accurate diagnosis.
While there is no known cure for Sjogren’s syndrome, there are various treatment options available to manage the symptoms and improve the quality of life for those living with this condition.
Symptomatic relief
The primary goal of treatment is to alleviate the symptoms associated with Sjogren’s syndrome, such as dryness of the eyes and mouth. Artificial tears and saliva substitutes can provide temporary relief by lubricating the affected areas. Medications like pilocarpine and cevimeline can stimulate tear and saliva production, while oral rinses and gels can help moisturize the mouth.
Joint and muscle pain management
Sjogren’s syndrome often leads to joint and muscle pain similar to that experienced in conditions like rheumatoid arthritis. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to manage pain and reduce inflammation. In more severe cases, corticosteroids may be prescribed to suppress the immune system and minimize the damage to joints and organs.
Dry skin treatment
Dry skin is a common symptom of Sjogren’s syndrome. Moisturizers and emollients can help to hydrate the skin and alleviate dryness. Protecting the skin from excessive sun exposure is also essential, as individuals with Sjogren’s syndrome are more prone to developing sunburn and other skin conditions.
Lubrication for other affected organs
In addition to the eyes and mouth, Sjogren’s syndrome can affect other organs, such as the lungs, kidneys, and digestive system. Depending on the severity of the symptoms, different medications can be prescribed to manage these complications and prevent further damage.
Pain management and rehabilitation
For individuals experiencing chronic pain and physical limitations, physical therapy and rehabilitation can be beneficial. These therapies aim to improve joint mobility, strengthen muscles, and reduce pain and discomfort.
Immunosuppressive therapy
In severe cases where Sjogren’s syndrome leads to significant organ involvement, doctors may prescribe immunosuppressive drugs. These medications suppress the overactive immune response that damages tissues and organs, providing relief and preventing further complications.
Lifestyle adjustments
Making certain lifestyle adjustments can also help manage the symptoms of Sjogren’s syndrome. These include drinking plenty of water, avoiding environmental factors that may worsen symptoms (such as smoke and dry environments), and practicing good dental hygiene to prevent tooth decay and gum disease.
Exploring Hashimoto’s and hypothyroidism
Your thyroid produces thyroid hormones that regulate metabolism, body temperature, and growth and development. Sometimes, your thyroid makes too much or too little thyroid hormone. As a result, thyroid disorders appear.
When you have an overactive thyroid, it produces too much thyroid hormone, resulting in hyperthyroidism. In contrast, an underactive thyroid produces too little thyroid hormone, resulting in hypothyroidism. Because of this, your body systems slow down, causing symptoms such as:
- Constipation
- Dry skin and hair
- Weight gain
- Cold intolerance
- Muscle aches
Autoimmune thyroid disorders (AITD)
While there are many potential causes of a thyroid disorder, one common cause is an autoimmune condition. The two most common autoimmune thyroid diseases are Graves’ disease and Hashimoto’s thyroiditis. Graves’ disease typically results in hyperthyroidism, while Hashimoto’s causes hypothyroidism.
Hashimoto’s
Hashimoto’s thyroiditis is the number one cause of hypothyroidism in the United States. Like Sjogren’s syndrome, your immune system mistakenly attacks healthy cells. But instead of your exocrine glands, with autoimmune thyroiditis, your immune system attacks your thyroid. As your immune system attacks your thyroid gland, thyroid hormone production decreases over time, resulting in hypothyroidism.
Individuals with Hashimoto’s often experience the same symptoms as those with hypothyroidism not caused by Hashimoto’s. The primary way to tell if someone has Hashimoto’s hypothyroidism is by the presence of specific thyroid antibodies.
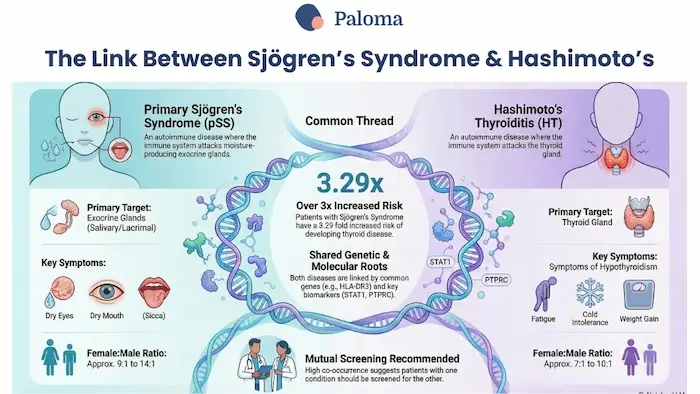
The key to the relationship between Sjogren’s syndrome and Hashimoto’s hypothyroidism is the autoimmune connection.
We have already established that both Sjogren’s syndrome and Hashimoto’s are autoimmune diseases. And it is well known that having one autoimmune condition puts you at risk for developing other autoimmune diseases.
Sjogren’s syndrome is more prevalent among those with Hashimoto’s compared to individuals with Graves’ disease. Individuals with Hashimoto’s are nearly four times more likely to develop Sjogren’s syndrome than those without Hashimoto’s.
A diagnosis of Sjogren’s syndrome can either come before or after the diagnosis of an AITD. However, one study found that in over half of those with Sjogren’s syndrome, an AITD was diagnosed on average 5.5 years later.
Here are three ways that literature supports the autoimmune disease connection between Sjogren’s syndrome and AITD.
1. Antibodies
Your immune system produces antibodies to help fight foreign invaders, like germs, that enter your body. Antibodies allow for quick recognition and destruction of foreign invaders before they can do any harm.
In an autoimmune disorder, the immune system goes rogue and develops autoantibodies against your healthy cells. These antibodies either destroy your cells or make them work overtime. In both cases, your cells are no longer functioning properly, thus affecting your overall body function.
Those with Hashimoto’s commonly have two thyroid-related autoantibodies in their blood: thyroglobulin (TG) and thyroid peroxidase antibodies (TPO). Research shows that individuals with Sjogren’s syndrome have higher levels of TG and TPO antibodies compared to those without Sjogren’s syndrome. The presence of thyroid antibodies in those with Sjogren’s syndrome is a significant risk factor for developing an AITD. Studies show the general prevalence of Sjogren’s syndrome in individuals with an AITD ranges from 3 to 32%.
2. Genetics
Research shows that individuals with Sjogren’s syndrome and autoimmune thyroiditis share similar genetic backgrounds. This means they have some common genetic markers, making individuals with specific genes more prone to either medical condition.
But, experts believe genetics only play a small part in the development of autoimmune diseases. Many believe it is a combination of genetics and environmental factors that trigger an autoimmune disorder.
3. Inflammatory markers
Your immune system is one of the driving forces behind inflammation in your body. In response to an injury or infection, your immune system boosts its production of inflammatory cells. In those with an autoimmune disorder, inflammation is chronic and ongoing. As a result, your immune system continues to send inflammatory cells and cytokines, a type of protein that promotes the production of more inflammatory cells, to that area.
Researchers have found that a specific inflammatory cytokine called CXCL10 is a strong marker for an aggressive inflammatory response. This is especially true in those with autoimmune thyroid disease. As a result, thyroid destruction occurs, leading to hypothyroidism. In addition, epithelial cells from individuals with Sjogren’s syndrome produce CXCL10 along with other cytokines, which contribute to salivary gland damage. Thus, the production of CXCL10 in those with Sjogren’s syndrome may result in thyroid damage and vice versa, further supporting the link between these two medical conditions.
For the population of patients living with both health conditions, it’s essential to manage them effectively. Here are some strategies to help navigate this dual challenge.
1. Regular check-ups: Regular follow-up appointments with your healthcare provider are vital. They can monitor your symptoms, adjust your treatment plan, and guide you on managing symptoms.
2. Medication management: Most people with Sjogren’s syndrome and hypothyroidism are prescribed medication to manage their symptoms. Unfortunately, each condition will likely need treatment with different medications, as no single medication treats both. Underactive thyroid disease in patients is managed by taking a daily thyroid hormone replacement medication. On the other hand, medications chosen to treat Sjogren’s syndrome vary based on symptoms.
3. Lifestyle changes: Making lifestyle changes such as improving your sleep or evaluating your diet are helpful for anyone with an autoimmune disorder. These lifestyle changes won’t reverse the damage already done but can prevent further damage and lessen your symptoms.
As mentioned, regular check-ups with your healthcare providers are essential for managing your symptoms of hypothyroidism. During these visits, your healthcare provider may check your thyroid function.
If this is your first time having your thyroid function tested, your provider will likely test for the three most common thyroid biomarkers - TSH, free T4, and free T3 - and TPO antibodies. The presence of thyroid antibodies doesn’t assess how well your thyroid functions. However, it will tell your provider if an autoimmune disorder like Hashimoto’s is the cause of your thyroid dysfunction.
Patients with thyroid disorders can check thyroid biomarkers in two ways: a blood draw at a lab or doctor’s office, or with an at-home testing kit. Paloma’s at-home testing kit only requires a finger prick blood sample to measure your thyroid biomarkers and TPO antibody levels. You will have your results within a week of mailing your test kit to the lab. And Paloma’s results come with a detailed explanation of what your levels mean.
The treatment approach for overt Hashimoto’s and hypothyroidism is the same. But, being aware of your autoimmune condition enables your healthcare provider to proactively screen for signs of other autoimmune disorders, such as Sjogren’s syndrome.
%20(1).webp)
.webp)













