In this article
Meet the experts
- Dr. Asimah Hanif is a UK-based physician and a member of the Royal College of General Practitioners (MRCGP).
- Nicholas Dragolea, MD, GP is a London-based general practitioner with a focus on longevity and functional health and founder of My Longevity Centre.
Living with hypothyroidism or another thyroid condition? You probably already know it can put the brakes on your energy, metabolism, and mood. But here’s something you may not expect—your thyroid could also be affecting your hearing! Surprising, right? Research shows a strong link between thyroid dysfunction and hearing loss, ringing in the ears (tinnitus), and even balance issues. In this article, we’re looking at the most common questions about how your thyroid health could be affecting your hearing—and what you can do about it.
Thyroid diseases—primarily hypothyroidism (an underactive thyroid) and hyperthyroidism (an overactive thyroid)—are increasingly recognized as important contributors to hearing disorders, including both hearing loss and tinnitus (commonly described as ringing, buzzing, or hissing in the ears). Thyroid hormones, especially thyroxine (T4) and triiodothyronine (T3), play a critical role in the growth, development, and maintenance of the entire auditory system, from the earliest stages of fetal development through adult life. Their influence extends to the sensory hair cells of the cochlea, myelination (insulation) of the auditory nerve, as well as the overall blood supply and metabolic support of the ear structures.
Epidemiological studies consistently demonstrate a higher risk of hearing impairment among those with hypothyroidism. For example, data suggest that people with hypothyroidism have nearly a 1.7-fold increased risk of any hearing loss compared to people who are euthyroid (normal thyroid function). And, up to 24% of people with hypothyroidism may exhibit measurable hearing impairment, a rate significantly above that of the general population.
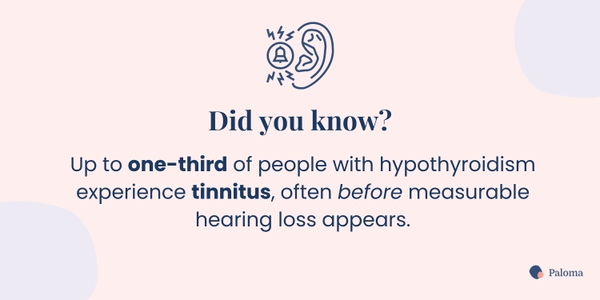
Similarly, tinnitus is a frequent and debilitating symptom in this group, occurring in up to one-third of patients with diagnosed hypothyroidism. Both overt and mild thyroid disturbances are now considered independent risk factors for hearing problems, and persistent tinnitus is reported by a large proportion of patients even before significant hearing loss is measurable.
What’s going on? When thyroid hormone levels are unbalanced—either too low (hypothyroidism) or too high (hyperthyroidism)—several mechanisms may impair hearing:
- Vascular effects: The cochlea is highly sensitive to changes in blood supply. Thyroid dysfunction can lead to constricted or poorly regulated blood flow, starving the inner ear of oxygen and nutrients.
- Neural conduction disruption: Low levels of thyroid hormone affect the insulation of auditory nerves, causing delayed or incomplete transmission of sound signals from the ear to the brain.
- Autoimmunity: In autoimmune disorders such as Hashimoto's thyroiditis and Graves’ disease, the immune system can attack elements of the inner ear, leading to inflammation and progressive damage.
Thyroid disease does not cause a single pattern of hearing impairment; instead, a number of distinct (and sometimes overlapping) types of hearing loss are seen in thyroid patients.
Sensorineural hearing loss (SNHL)
This is by far the most prevalent—accounting for approximately 90% of hearing loss both in the general public and in people with thyroid disorders. SNHL reflects damage to the hair cells in the cochlea and/or the auditory nerve pathways. In hypothyroidism, researchers have found:
- Both bilateral (both ears) and unilateral losses can occur.
- The loss can affect all frequencies, but high-frequency loss (trouble hearing high-pitched sounds) is especially common.
- In children born to mothers with untreated hypothyroidism, congenital SNHL may result.
Conductive hearing loss (CHL)
CHL occurs when the pathway transmitting sound from the external environment into the inner ear is blocked or impaired. In patients with hypothyroidism, a frequent cause is the build-up of thick, sticky earwax (cerumen)—partly due to slower metabolism and glandular secretions. Fluid behind the eardrum (known as middle ear effusion) has also been reported, more so in younger patients or those with severe hormone deficiency.
Sudden sensorineural hearing loss (SSNHL)
This is a dramatic, rapid loss of hearing—sometimes affecting only one ear, and occurring over a period of 72 hours or less. Research shows that patients with hypothyroidism, particularly those over age 50, are at increased risk of SSNHL, a condition requiring immediate medical evaluation. Treatment delay may lead to permanent deafness.
Autoimmune inner ear disease (AIED)
For individuals with autoimmune thyroid conditions such as Hashimoto’s, the body’s immune cells sometimes cross-react with and attack components of the inner ear. Symptoms typically include progressive or fluctuating hearing loss (in one or both ears), persistent tinnitus, and episodes of imbalance or vertigo. Autoimmune inner ear disease (AIED) may result in permanent hearing impairment if left untreated.
Meniere’s disease
There is a distinctly higher prevalence of Meniere’s disease in patients with Hashimoto’s thyroiditis and hypothyroidism, according to recent epidemiological surveys. Meniere’s disease is characterized by episodes of spinning vertigo, roaring tinnitus, ear fullness, and varying degrees of hearing loss. The strong autoimmune disease link in both conditions suggests a shared origin.
The symptoms of thyroid-related hearing loss can be subtle at first but often worsen over time if thyroid status remains unaddressed. Below are typical manifestations to watch for:
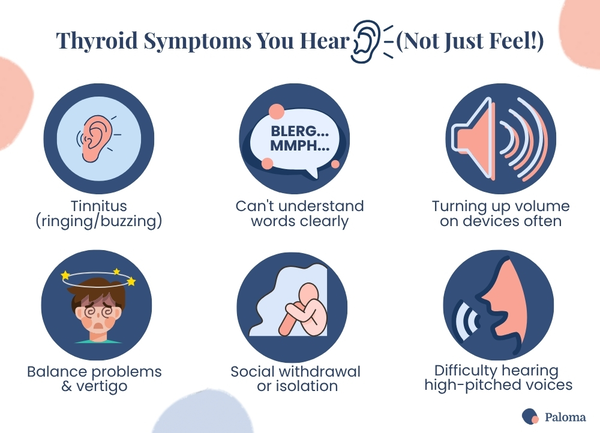
Tinnitus
Tinnitus is described as persistent or intermittent sounds (ringing, buzzing, hissing, or roaring) without external sources. For many, tinnitus is the earliest and most distressing symptom.
Problems understanding speech
Patients frequently report the ability to “hear” sounds but not “understand” words, especially in group conversations or environments with background noise (the “cocktail party” effect). Difficulty following phone conversations is common.
- Volume increase: Repeatedly turning up the TV, radio, or phone, or asking people to repeat themselves; often, this doesn't make words clearer, only louder.
- Ear fullness/pressure: Dr. Nicholas Dragonlea says his patients sometimes describe “a feeling of fullness or pressure, like their ears are blocked.” These symptoms may sometimes be mistaken for sinus or allergy symptoms.
- Difficulty with certain voices: Struggling to distinguish higher-pitched voices (women, children) or certain consonants, such as “s,” “th,” or “f.”
- Balance problems: Episodes of dizziness, vertigo, unsteadiness, or even falls—especially relevant for seniors and those with Meniere’s or AIED.
- Prolonged onset: Gradual progression, leading patients to adapt or compensate before seeking help, which can delay diagnosis and effective treatment.
- Reduced participation: Becoming socially withdrawn, frustrated, or anxious about communication in group settings due to hearing difficulties.
Early recognition of such symptoms, especially in those with known thyroid disease, is crucial for prompt intervention and improved quality of life.
The relationship between thyroid treatment and auditory recovery is nuanced but generally encouraging, especially if intervention is timely:
Medication response
In cases where hearing impairment or tinnitus is directly attributable to hypothyroidism, normalization of thyroid hormone levels with synthetic levothyroxine or other thyroid hormone preparations can lead to significant, sometimes total, symptomatic improvement. Several clinical studies reveal that after 6 to 12 months of optimal thyroid hormone therapy:
- Nearly half (up to 50%) of hypothyroid patients with hearing problems notice meaningful improvement.
- Roughly 15% of sufferers experience complete resolution of symptoms, especially if intervention is early.
According to Dr. Asimah Hanif, "Treating the underlying thyroid issue — especially with thyroid hormone replacement in hypothyroidism — can sometimes improve hearing and reduce tinnitus, especially if caught early. But it’s not guaranteed. If the hearing loss is due to long-term damage, hormone treatment may stabilize the issue, rather than reverse it."
Variable outcomes
Some individuals continue to struggle with persistent tinnitus or incomplete hearing recovery even after thyroid labs are “normal.” This may result from delayed treatment, autoimmune damage, or irreversible nerve/cellular injury.
Medication side effects
Rarely, patients starting or adjusting to high doses of thyroid hormone replacement report onset or worsening of tinnitus. This effect is usually transient and resolves as hormone levels stabilize.
Comprehensive care
Achieving optimal—not just “laboratory normal”—thyroid levels is vital, as symptom relief correlates more closely with individually optimized dosage than with generic reference ranges. Co-management of cardiovascular risk, blood pressure, and metabolic complications can further enhance outcomes.
Management of coexisting factors
Addressing coexistent anxiety, insomnia, and other medical problems can also alleviate tinnitus and improve hearing outcomes.
Hearing screening and proactive monitoring are essential components of comprehensive thyroid care.
Routine checks: If all is stable and there are no hearing issues, testing every 2 to 3 years is reasonable — sooner if symptoms pop up.":
- Initial baseline test: Seek a hearing evaluation (comprehensive audiogram) as soon as possible after a diagnosis of hypothyroidism, Hashimoto's, or any other thyroid disease; this provides a valuable reference to judge subsequent changes.
- Annual or biannual checks: Audiology specialists typically recommend annual hearing re-checks, but at minimum, patients should be retested every two years, even in the absence of new symptoms.
- Self-assessment: Utilize an online hearing test (such as this one from United Health Care) for informal self-checks between visits. Note any declines or new symptoms for prompt reporting to your provider.
- Urgent evaluation: Any new, sudden, or severe decrease in hearing, especially over a span of hours or days (as with SSNHL), is a genuine medical emergency. Immediate referral to an ENT specialist may make the difference between complete recovery and permanent loss.
- Other indications for referral: Rapid development of severe tinnitus, dizziness, vertigo, or loss of balance warrants urgent evaluation.
According to Dr. Asimah Hanif, you should also have a hearing retested “if your thyroid levels fluctuate or if you develop new hearing issues or tinnitus. If all is stable and there are no hearing issues, routine testing every 2 to 3 years is reasonable — sooner if symptoms pop up.”
Proactive hearing health preserves communication, independence, and safety—especially important as thyroid disorders frequently affect women, older adults, and individuals at higher risk for multiple health problems.
An audiological assessment is straightforward, non-invasive, and informative. The process usually takes 30 to 45 minutes and includes several components:
- Detailed medical history: The audiologist will ask about thyroid status, medications, past ear infections, noise exposure, and other health factors that could affect hearing.
- Otoscopic examination: Using a lighted instrument, the provider visually inspects your ear canals for blockages (e.g., wax), inflammation, or abnormalities. Professional wax or object removal may be performed as needed—never use cotton swabs (“Q-tips”), which can compact wax and worsen blockages.
- Tympanometry: A small probe, temporarily placed in the ear, measures eardrum movement and middle ear pressure to detect fluid, infection, and eustachian tube dysfunction.
- Pure-tone audiometry: Wearing earphones, you respond to tones of varying frequencies and volumes. The softest level at which you can reliably detect sound at each pitch is recorded to form a graph (an audiogram).
- Bone conduction testing: Using a vibrating oscillator placed behind the ear, this test bypasses the outer and middle ear to evaluate the inner ear's health; discrepancies with air conduction results help pinpoint the location of impairment.
- Speech understanding tests: You’ll be asked to repeat spoken words or sentences in quiet and in background noise. More advanced tests may assess how your brain processes complex speech, guiding hearing aid or rehabilitation recommendations.
- Results and counseling: The audiologist reviews your results, discusses patterns (e.g., frequency-specific loss), and provides both treatment recommendations and educational resources.
Patients with thyroid disorders benefit from having both their audiologist and thyroid specialist collaborate to optimally interpret results and tailor follow-up.
Individualized, patient-centered care is crucial. Coordination between endocrinologists, ENTs, audiologists, and primary care physicians produces the best outcomes, especially for those with autoimmune or complex multisystem involvement.
The appropriate management depends on the type and severity of the hearing loss.
Sudden sensorineural hearing loss
SSNHL constitutes an emergency. High-dose oral corticosteroids (e.g., prednisone) may be initiated to reduce inflammation and preserve or restore hearing, alongside further examination to exclude infections, tumors, or autoimmune processes.
Conductive hearing loss
Many cases are readily treated by medical or minor surgical interventions, including:
- Removal of excessive earwax (cerumen) or foreign objects.
- Drainage of fluid or treatment of middle ear infections (with or without pressure equalization tubes for chronic cases).
- Attention to allergies or sinus issues, which may contribute to temporary blockage.
If medical measures do not resolve the issue, hearing aids may help overcome residual conductive deficits.
Sensorineural hearing loss
The mainstay is aural rehabilitation, including:

- Hearing aids: Available in various styles (in-the-ear, behind-the-ear, open-fit, etc.), these devices can be fine-tuned to each individual’s pattern and severity of loss. Many modern aids also provide tinnitus-masking functions.
- Cochlear implants: For severe or profound SNHL, surgically implanted devices may restore usable hearing, though candidacy depends on several factors.
Mixed hearing loss
Combined management strategies are used, often involving both medical/surgical and audiological interventions.
Tinnitus management
- Sound therapy (background white noise machines, ocean or rainfall sounds, or specialized tinnitus maskers).
- Hearing aids tailored to amplify speech while minimizing tinnitus perception (especially for those with concurrent hearing loss).
- Cognitive behavioral therapy and psychological support for severe distress or insomnia secondary to tinnitus.
- Lifestyle modifications: Avoidance of silence, stress reduction, and prioritizing sleep hygiene all reduce overall tinnitus impact.
- Thyroid optimization: Addressing any underlying thyroid imbalance is critical, as symptom improvement is often directly linked to normalization of thyroid hormone levels.
Some types of hearing loss are not preventable (for example, those caused by genetics, congenital anomalies, autoimmune damage, or aging). According to Dr. Hanif, you can reduce your risk in several ways.
Hearing protection
The most important controllable factor for everyone is noise exposure. Wear properly-fitted ear protection during loud activities (concerts, sporting events, power tools, workplace machinery). Even “temporary” ringing after loud sounds is a warning that hearing cells are being damaged.
Be careful when using earbuds and headphones
To protect your hearing when using earbuds or headphones, keep the volume at 60% or lower and limit listening sessions to no more than 60 minutes at a time—the “60/60 rule.” Noise-canceling headphones can help reduce the temptation to turn up the volume in noisy environments. Avoid using earbuds in loud places like airplanes, gyms, or on public transit where background noise can make you crank the volume higher without realizing it. Over-the-ear headphones are generally safer than in-ear models because they sit farther from the eardrum. Also, be sure to take listening breaks throughout the day to give your ears a rest and allow time to recover.
Thyroid optimization
Proactive, ongoing management of thyroid health through regular testing and monitoring, optimal medication management, dietary support, and treatment of other related medical issues helps prevent or stabilize progressive hearing impairment.
Dr. Nicholas Dragolea stresses the importance of this component of thyroid care. “Patients with thyroid conditions can certainly take steps to minimize the risks of hearing loss. Optimizing their thyroid control is beneficial, and this involves regular monitoring of their thyroid levels and titrating the medication accordingly. Improving thyroid hormone levels increases the blood flow in the inner ear again, and studies have shown that this can improve or even reverse hearing loss and tinnitus.”
Regular screening
Annual (or, at minimum, biennial) hearing assessments, starting at diagnosis, allow for detection of early changes—empowering patients to initiate treatment while hearing loss is still treatable.
Prompt medical attention
Never delay seeking care for new, sudden, or rapidly worsening hearing problems. Immediate assessment may enable medical interventions that save or recover hearing, especially in cases of SSNHL or autoimmune inner ear attacks. Dr. Dragolea agrees. “Any new decrease in hearing or tinnitus should prompt an early review by a healthcare professional for the highest chance of preventing hearing loss.”
Safe earwax management
Hypothyroid patients with a history of earwax buildup should avoid cotton swabs, bobby pins, ear candles, or other methods to extract wax. Discuss safe removal methods with your physician or audiologist, including use of over-the-counter drops (like Debrox) or scheduled in-office cleanings.
Healthy lifestyle choices
- Avoid smoking and secondhand smoke, which can impair blood flow to the inner ear.
- Control high blood pressure, cholesterol, and diabetes, as these conditions also damage auditory blood vessels.
- Practice good sleep habits and manage stress, as anxiety and insomnia can worsen tinnitus.
- Stay hydrated and maintain a nutritious, anti-inflammatory diet to support thyroid and systemic health.
Hearing loss and tinnitus may not be the first symptoms that come to mind when you think about thyroid disease—but they deserve your attention. Whether you're dealing with frustrating ringing in your ears or struggling to understand conversations, these signs may be more than just "getting older." Don't assume that you're experiencing age-related hearing loss.
Instead, when you recognize the connection between your thyroid and hearing health, you can take proactive steps to protect your quality of life and stay engaged in the world around you. And the good news? You don’t have to do it alone!
At Paloma Health, we believe that thyroid care should go beyond lab tests and symptoms checklists. Paloma members benefit from a whole-body approach—because your thyroid impacts every system, including your ears. Our expert providers specialize in personalized thyroid care, helping you optimize your hormone levels, manage complex symptoms, and feel like yourself again. And Paloma’s convenient home thyroid test kit makes it easy to stay on top of thyroid levels and hypothyroidism treatment.
If you’re experiencing hearing changes, tinnitus, or balance issues, we’re here to help you connect the dots and find solutions. With comprehensive care, you don’t just live with thyroid disease—you thrive. Book your appointment today and let’s work together on your journey to better health.
🔊 Thyroid hormones are essential for hearing health. Imbalances in thyroid hormones can disrupt blood flow, nerve signaling, and inner ear function, leading to hearing problems.
👂 Thyroid disease can cause different types of hearing loss. People with thyroid issues may experience sensorineural, conductive, sudden, or autoimmune-related hearing loss.
🔔 Tinnitus is a common thyroid-related symptom. Ringing or buzzing in the ears often appears early in thyroid dysfunction, especially with hypothyroidism or Hashimoto’s.
💊 Treating your thyroid can improve hearing symptoms. Normalizing thyroid hormone levels can lead to partial or full recovery of hearing and reduce tinnitus in many cases.
📅 Regular hearing checks are important for thyroid patients. Baseline and follow-up audiograms help detect changes early and guide timely treatment.
🎧 Many hearing loss treatments are available. Depending on the cause, options may include thyroid medication, hearing aids, sound therapy, or medical procedures.

.webp)
.webp)











