In this article
Few symptoms are as instantly alarming as heart palpitations.
One moment your heart feels normal — the next it’s fluttering, pounding, or skipping beats. For people with thyroid problems, these sensations are especially common, particularly with overactive thyroid function or too much thyroid medication. Understanding what’s happening inside your body, what can set palpitations off, and when they require medical attention can replace fear with confidence — and help you respond instead of panic.
Heart palpitations are the sensation of being suddenly aware of your heartbeat, even though your heart is always beating in the background. They can show up when you are resting quietly, falling asleep, exercising, or even out of the blue.
Common ways people describe palpitations include:
- A fluttering or “butterflies in the chest” feeling.
- A racing heartbeat, like your heart is pounding out of your chest.
- Hard, forceful thumps or “extra beats,” sometimes followed by a pause.
- A flip-flop or “dropped beat,” often with a brief “catching your breath” feeling.
Palpitations can be brief (a second or two), last several minutes, or come and go in waves over hours. Severity is less about how dramatic they feel and more about what the underlying rhythm is and whether there are concerning symptoms, such as:
· Chest pain or pressure.
- Shortness of breath or trouble catching your breath.
- Dizziness, feeling faint, or actually passing out.
- New swelling in your legs, sudden fatigue, or exercise intolerance.
Any palpitations accompanied by those red-flag symptoms require immediate medical evaluation or emergency care.
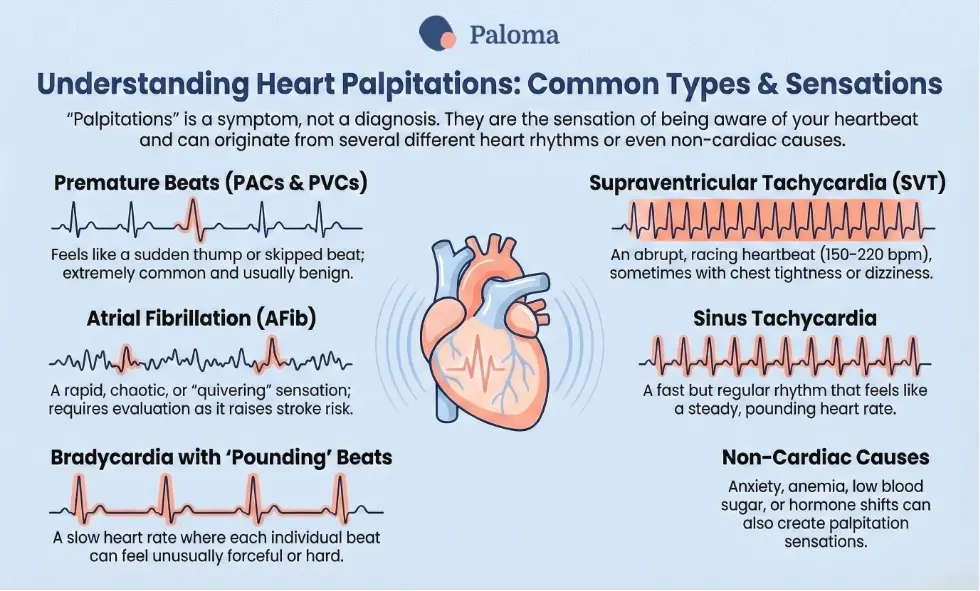
“Palpitations” are a symptom, not a diagnosis. They can come from several different heart rhythms or even from non-cardiac causes. Here are some of the more common patterns.
Premature beats (PACs and PVCs)
- Premature atrial contractions (PACs) and premature ventricular contractions (PVCs) are early heartbeats that interrupt the normal rhythm.
- They often feel like a sudden strong thump, a skipped beat, or a brief flutter, then everything returns to normal.
- These types of palpitations are extremely common and usually benign in an otherwise healthy heart. However, they can be more noticeable when you are stressed, when you use caffeine, or when your thyroid is overactive.
Supraventricular tachycardia (SVT)
- SVT is a rapid heartbeat that starts in the upper chambers (atria) of the heart, usually with rates of 150–220 beats per minute.
- You may feel an abrupt “on/off” racing heartbeat, sometimes with chest tightness, shortness of breath, or lightheadedness.
- SVT episodes may stop on their own, respond to “vagal maneuvers” (see below), or require medication.
Atrial fibrillation (AFib)
- AFib is an irregular, often fast rhythm arising from disorganized electrical activity in the atria.
- Palpitations can feel like a rapid, chaotic, or “quivering” heartbeat rather than a smooth rhythm.
- Atrial fibrillation is linked explicitly with hyperthyroidism and overmedication with thyroid hormone and requires evaluation because it raises stroke risk.
Sinus tachycardia
- This is a fast but regular rhythm from the heart’s normal pacemaker (the sinus node).
- It can be an appropriate response (exercise, fever, anxiety) or inappropriate (overactive thyroid, certain medications, dehydration).
- Many people feel this as a steady, pounding fast heart rate, especially at rest or when lying down.
Bradycardia with “pounding” beats
- Hypothyroidism often causes a slow heart rate (bradycardia), but some people still notice occasional hard beats or awareness of their heart, particularly with exertion.
- The slower rhythm can make each beat feel more forceful.
Non-cardiac causes—like anxiety, panic attacks, anemia, low blood sugar, or hormone shifts—can also produce palpitations or make normal beats feel overly intense.
Thyroid hormones directly affect how fast and how forcefully your heart beats, as well as how responsive it is to adrenaline-type signals. When your thyroid levels are off—either too high or too low—heart rhythm can be one of the first things you notice.
Hyperthyroidism (overactive thyroid)
- Too much thyroid hormone speeds up metabolism, increases your resting heart rate, and makes the heart more irritable electrically.
- Common symptoms of hyperthyroidism include palpitations, anxiety, heat intolerance, sweating, tremor, weight loss, and sometimes shortness of breath or chest discomfort.
- An irregular or unusually fast heart rate is a classic sign of hyperthyroidism and should always prompt thyroid testing.
Hypothyroidism (underactive thyroid)
- Low thyroid hormone slows metabolism and typically lowers your heart rate (bradycardia).
- You may feel tired, cold, short of breath on exertion, or dizzy if your heart rate is very slow.
- Palpitations can still occur (for example, from premature beats), but are less likely to be from very fast rhythms in hypothyroidism.
Overmedication with thyroid hormone
- Taking more thyroid hormone replacement medication than your body needs can push you into “iatrogenic” or medication-induced hyperthyroidism.
- Signs include a racing heartbeat, palpitations, anxiety, tremor, insomnia, weight loss, and sometimes elevated blood pressure.
- Even mild over-replacement—where blood tests show low TSH but T3/T4 are in the normal range—can increase the risk of atrial fibrillation and other arrhythmias.
Because of these effects, any new-onset palpitations in someone with known thyroid disease (or on thyroid medication) should prompt a careful review of thyroid labs and dosing.
Gut health and medication timing can indirectly trigger palpitations by pushing thyroid hormone levels too high or too low.
Absorption issues and dose swings
- Conditions like celiac disease, inflammatory bowel disease, autoimmune gastritis, H. pylori, or atrophic gastritis can change how well your thyroid medication is absorbed, causing unstable levels.
- Taking your thyroid medication too close to calcium, iron, high-fiber meals, some antacids, or proton pump inhibitors can reduce absorption—or correcting these habits may suddenly increase absorption and temporarily overshoot, leading to palpitations.
Weight loss or diet changes
- Significant weight loss, bariatric surgery, or very low-calorie diets can make a once-appropriate thyroid dose too high, resulting in palpitations and other hyperthyroid symptoms.
- Conversely, gaining weight without adjusting thyroid medication may contribute to persistent hypothyroid symptoms and fatigue, sometimes with awareness of slow or forceful heartbeats.
GI distress and the autonomic nervous system
- Bloating, reflux, and IBS-type symptoms can increase your awareness of palpitations because the gut and heart share nervous system pathways, especially via the vagus nerve.
- When your gut is irritated, discomfort and anxiety can amplify normal heart sensations.
If palpitations started after a change in medication brand, timing, diet, or digestive health, that timeline is essential to share with your clinician.
Diet is a frequent and often fixable trigger for palpitations. Common food and drink triggers include:
Caffeine
- Coffee, energy drinks, strong tea, pre-workout powders, and some sodas can increase your heart rate and make premature beats more noticeable.
- People with hyperthyroidism or on high-normal thyroid doses are often more sensitive to these stimulants.
Alcohol
- Alcohol can provoke atrial fibrillation in susceptible people—sometimes called “holiday heart”—and also disrupts sleep, which itself raises the risk of palpitations.
- Binge drinking is particularly associated with episodes of irregular heartbeat.
Sugar and refined carbohydrates
- Large, high-sugar meals can cause swings in blood sugar and adrenaline, which may feel like a racing heart, shakiness, or anxiety.
- In some people, especially those with reactive hypoglycemia or insulin resistance, these swings can be misread as “thyroid” symptoms.
High-sodium or ultra-processed foods
- Salty fast food, processed meats, and packaged snacks can raise blood pressure and fluid retention, increasing workload on the heart.
- People with underlying heart disease, AFib, or hyperthyroidism may be especially sensitive.
Acidic foods and drinks
- Acidic items like citrus, tomatoes, coffee, and sodas worsen reflux, mimicking palpitations with chest fluttering.
- Esophageal irritation from reflux stimulates nearby nerves, heightening heartbeat awareness or brief rhythms.
- Large acidic meals distend the stomach, pressing the diaphragm and causing post-meal pounding.
- Caffeinated acidic drinks (coffee, cola) boost heart rate, amplifying symptoms.
- Acidic alcohol (wine, citrus cocktails) aggravates reflux and disrupts heart signals.
Food sensitivities and histamine-rich foods
- In susceptible individuals, histamine-rich foods (aged cheeses, wine, fermented foods) or allergies can cause flushing, palpitations, or a sense of internal “revving.”
Keeping a simple symptom and food diary for 1–2 weeks can help you spot patterns between your meals, drinks, and palpitations, especially when you overlay thyroid medication timing and stress levels.
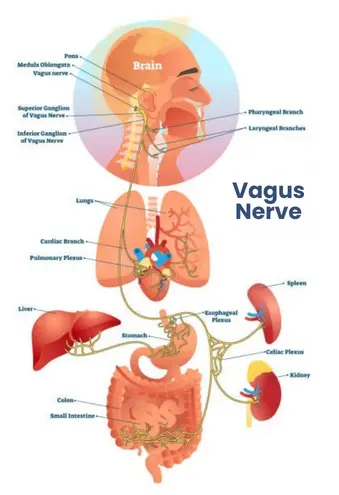
The vagus nerve is part of the parasympathetic (“rest-and-digest”) system and helps regulate your heart rate, gut motility, and many internal organs. Sometimes, palpitations are related to changes in vagal tone rather than a primary heart problem.[ncbi.nlm.nih]
What “vagal” palpitations feel like
- You may notice palpitations when you’re bending over, straining at stool, coughing, or after a big meal—situations that stimulate your vagus nerve or change pressure in the chest.
- You may also feel a sudden pause or heavy beat after swallowing or with reflux, again reflecting gut–heart nerve interactions.
Vagal maneuvers as a treatment tool
- Clinicians use “vagal maneuvers” to intentionally stimulate the vagus nerve and slow certain fast rhythms, especially SVT.
- Examples include the Valsalva maneuver (bearing down as if having a bowel movement), coughing forcefully, or, in medical settings, carotid sinus massage.
- These maneuvers can sometimes stop an SVT episode. Still, they should be taught and supervised by a clinician because they are not appropriate for everyone (e.g., people with carotid artery disease).
In everyday life, practices that support a calmer autonomic nervous system—such as slow breathing, gentle yoga, and stress-reduction techniques—can also reduce vagally related palpitations for many people.
A careful evaluation examines both the heart rhythm itself and underlying triggers, such as thyroid disease, anemia, or structural heart problems. The following are the typical steps in the evaluation:
Detailed history and physical exam
- Your clinician will ask when palpitations started, what they feel like, how long they last, what triggers or relieves them, and any associated symptoms.
- They will also review your medications (including thyroid hormone), supplements, caffeine and alcohol intake, and family history of heart disease.
Electrocardiogram (ECG/EKG)

- A 12-lead ECG records the heart’s electrical activity over a few seconds and can identify active arrhythmias, conduction problems, prior heart damage, or signs of hyperthyroidism-related strain.
- Since palpitations are often intermittent, a normal ECG does not rule out an episodic rhythm problem.
Ambulatory monitoring
- Holter monitors (24–48 hours) or patch/event monitors (days to weeks) track heart rhythm over time and aim to capture an episode.
- For very infrequent but concerning palpitations, an implantable loop recorder may be used to monitor for months or years.
Blood work
- A thyroid panel to measure thyroid hormones – thyroid-stimulating hormone (TSH), free thyroxine (free T4), and free triiodothyronine (free T3) is essential when palpitations are present, especially if there are other thyroid symptoms.
- Labs may also check for anemia, electrolyte imbalances, kidney function, and markers of heart strain.
Imaging and further testing
- An echocardiogram (ultrasound of the heart) looks for structural problems (valve disease, cardiomyopathy, heart failure) that can predispose you to arrhythmias.
- In select cases, stress testing or an electrophysiology study may be recommended.
A key aim is to match the “symptom story” with an actual rhythm strip so your treatment is tailored to what is truly happening.
Treatment depends on the underlying rhythm and the overall risk profile, not just on how uncomfortable the palpitations feel. For thyroid-related palpitations, correcting thyroid hormone levels is foundational.
For hyperthyroidism or overmedication
- Antithyroid medications: Drugs like methimazole – or in some cases propylthiouracil (PTU) – reduce thyroid hormone production in hyperthyroidism, which gradually calms heart rate and palpitations.
- Beta-blockers: Medications such as propranolol, metoprolol, or atenolol slow the heart rate and blunt the effects of adrenaline, often providing rapid relief from palpitations, tremor, and anxiety while thyroid levels are being corrected. Beta-blockers may also be used temporarily in people overmedicated with thyroid hormone replacement therapy while the dose is adjusted.
- Adjusting thyroid hormone dose: When palpitations are due to taking too much thyroid medication, the main treatment is lowering the dose and rechecking labs after about 6–8 weeks. Many people notice palpitations improve as levels normalize, though it can take some weeks for your body to adapt fully.
For specific arrhythmias
- Premature beats (PACs/PVCs): If your heart is structurally normal, treatment may focus on reassurance, lifestyle changes (limiting caffeine, alcohol, stress), and correcting your thyroid or electrolyte imbalances. Beta-blockers are sometimes used if symptoms are very bothersome.
- SVT: Acute treatment in a medical setting may include vagal maneuvers and a rapid IV medication such as adenosine to interrupt the abnormal circuit. For recurrent SVT, daily medications (beta-blockers or calcium channel blockers) or catheter ablation (a procedure to destroy the tiny area causing abnormal signals) may be recommended.
- Atrial fibrillation: AFib management typically includes rate-control medications (beta-blockers, calcium channel blockers) and sometimes rhythm-control drugs or ablation. Depending on your stroke and heart health risk, blood thinners are often prescribed to prevent clot formation due to cardiac arrhythmias.
- Thyroid correction: Correcting hyperthyroidism or adjusting thyroid medication is crucial because ongoing thyroid excess can sustain AFib.
Medication choices always need to be individualized based on your age, blood pressure, other conditions, and potential drug interactions.
Holistic approaches do not replace medical evaluation—especially for new, severe, or worsening palpitations—but they can be powerful adjuncts that reduce both triggers and symptom intensity.
Foundational lifestyle steps
- Balance thyroid levels: Work with your clinician to keep TSH, free T4, and free T3 within a range where you feel well and your heart rate is comfortable. And take your thyroid replacement medication consistently on an empty stomach, and separate it from calcium, iron, and certain supplements by at least 4 hours to avoid absorption fluctuations.

- Optimize sleep and minimize stress: Poor sleep and chronic stress increase adrenaline and cortisol, both of which can raise your heart rate and make palpitations more frequent. Simple daily practices—10–15 minutes of slow breathing, gentle yoga, walking outdoors, or guided relaxation—can calm your autonomic nervous system and reduce vagally related palpitations.
- Exercise smartly: Regular, moderate exercise improves heart conditioning and can reduce resting heart rate over time. If palpitations worsen with intense workouts or you have known arrhythmias, your clinician may recommend a tailored exercise plan and, in some cases, a monitored stress test before ramping up.
Nutritional and supplement support
Always review supplements with your healthcare provider, as some can interact with medications or underlying heart conditions.
- Magnesium: Magnesium plays a role in the electrical stability of the heart and may help reduce benign palpitations in some people with low intake. You’ll find magnesium in leafy greens, nuts, seeds, and whole grains; supplements are sometimes used cautiously if kidney function is normal.
- Electrolyte balance: It’s important to get adequate potassium and magnesium from whole foods to support normal rhythm. Very low or very high levels (for example, from certain diuretics or supplements) can provoke arrhythmias.
- Anti-inflammatory eating pattern: Diets emphasizing vegetables, fruits, high-quality protein, omega-3 fats, and minimally processed foods support vascular and thyroid health and may indirectly reduce arrhythmia risk. Limiting ultra-processed foods and added sugars can also help stabilize blood sugar and reduce “adrenaline spikes.”
- Limit stimulants and alcohol: Reducing caffeine and energy drinks is often one of the simplest ways to improve palpitations, especially if your thyroid levels are high-normal. Moderating alcohol and avoiding binges also lower the chance of AFib episodes in prone individuals.
Mind–body and vagal-calming techniques
- Breathwork and relaxation: Slow, diaphragmatic breathing (for example, inhaling to a count of 4, exhaling to 6–8) can activate the parasympathetic system and help break the cycle of anxiety🡪 palpitations🡪 more anxiety. Mindfulness, meditation, or cognitive behavioral strategies can help you respond to palpitations with less fear, which often makes them feel less intense.
- Gentle movement: Restorative yoga, tai chi, and qigong blend movement with breath and have been associated with improved heart rate variability and lower perceived stress. These practices can be especially valuable for people with thyroid disease who are rebuilding exercise tolerance.
- Address gut–heart connections: Treating reflux, SIBO, IBS, or other gut issues may reduce vagal triggers and overall body “alarm” signals. Eating smaller, more frequent meals and avoiding lying flat right after eating can decrease both reflux and post-meal palpitations.
While many thyroid-related palpitations are benign and improve with dose adjustments and lifestyle changes, there are situations where immediate medical attention is critical. Call emergency services or go to the ER if:
- Palpitations are accompanied by chest pain, pressure, or tightness.
- You feel faint, actually pass out, or have severe shortness of breath.
- Your heart rate is persistently above about 150 beats per minute at rest, and you feel unwell.
- You have known heart disease or AFib and notice a sudden change in pattern, intensity, or associated symptoms.
For anyone with thyroid disease, the combination of new or worsening palpitations plus other symptoms—such as weight loss, tremor, heat intolerance, or anxiety—warrants a prompt check of thyroid labs and a conversation with a knowledgeable clinician.
Used thoughtfully, this information can help you track patterns, advocate for appropriate testing, and combine conventional and holistic strategies so that your heart and thyroid can work together—rather than against you—on the path back to feeling well.
Heart palpitations can feel alarming, especially if you have a thyroid condition. Your thyroid affects your metabolism, energy, and even your heart rhythm, so fluttering, skipped, or racing beats are not uncommon.
Most palpitations are harmless, often triggered by stress, caffeine, or diet—but sometimes they warrant a closer look. Tracking when they happen, what you were doing, and any other symptoms can be very helpful.
At Paloma, we’re here to support you. You can use easy at-home Paloma tests to monitor your thyroid levels, and our care team can help monitor your thyroid, guide lifestyle strategies, and adjust treatment if needed. As a Paloma patient, you can feel confident and in control of both your thyroid and your heart health!
Can thyroid medication cause palpitations?
Yes, over-replacement with thyroid hormone replacement drugs mimics hyperthyroidism, speeding heart rate and causing flutters; lowering the dose often resolves it within weeks.
Are palpitations from hyperthyroidism dangerous?
Usually not if caught early, but they raise AFib risk; beta-blockers provide quick relief, while treating the thyroid fixes the source.
How do acidic foods trigger palpitations?
Acidic foods worsen reflux, irritating esophageal nerves near the heart and mimicking or amplifying awareness of the heartbeat, especially post-meal.
What are vagal palpitations?
Vagal palpitations occur from gut pressure (bending, big meals) stimulating the vagus nerve, causing brief pauses or thumps; breathwork often helps.
How is the thyroid-gut link involved?
Poor absorption from IBS, SIBO, or gastritis leads to hormone swings; fixing gut issues stabilizes levels and reduces palpitations.
When should you go to the ER for palpitations?
Seek help for chest pain, fainting, severe shortness of breath, or rates over 150 bpm at rest—don’t wait if thyroid symptoms accompany them.
Do holistic treatments replace medications for palpitations?
No, but magnesium, stress reduction, and trigger avoidance complement meds, calming the nervous system and preventing episodes.
Can diet alone fix thyroid palpitations?
Diet helps by cutting caffeine/alcohol/acid, but thyroid labs and dose tweaks are essential first steps for lasting relief from palpitations.
Is AFib common with thyroid overmedication?
Yes, even mild excess thyroid hormone boosts AFib risk; prompt lab checks and adjustment prevent progression.




.webp)








