In this article
Why talk about hemorrhoids?
Let’s be honest—hemorrhoids aren’t exactly dinner table conversation. Most people would rather talk about just about anything else! And hypothyroidism? Or menopause? We’re talking about a whole different universe of sluggish metabolism, fatigue, and hormonal swings. But here’s the twist: they are actually connected!
In this article, we’ll explore the surprising ways an underactive thyroid – as well as the menopausal transition – can set the stage for hemorrhoids, explain the underlying mechanisms, and provide practical tips on prevention, treatment, and holistic health management. We’ll also look at what you can do to keep things moving—literally and figuratively—for better comfort and overall health.
Hemorrhoids are swollen or inflamed veins in the lowest part of your rectum and anus. They’re common and can cause discomfort, itching, and, sometimes, rectal bleeding. Hemorrhoids are often linked to increased abdominal pressure, straining during bowel movements, constipation, pregnancy, obesity, prolonged sitting, and low-fiber diets.
There are three different types of hemorrhoids:
- Internal hemorrhoids: Form inside the rectum; usually not visible or painful, but may cause bleeding.
- External hemorrhoids: Develop under the skin around the anus; can itch or bleed, and may be painful.
- Thrombosed hemorrhoids: When blood pools and forms a clot, causing severe pain, swelling, and inflammation.
The prevalence of hemorrhoids in the general population varies depending on the study and the methods used.
- Most large studies report that approximately 9–16% of adults worldwide are affected by hemorrhoidal disease at any given time, with around 11% being a widely cited average in many surveys.
- Epidemiological studies estimate that symptomatic hemorrhoids are present in about 4.4% of the general population.
- Some studies cite an even broader claim that, over a lifetime, up to 50–85% of people may experience hemorrhoids, including both symptomatic and incidental (asymptomatic)
In summary, hemorrhoids are common: about 1 in 10 adults have them at any one time, but up to half or more of people may suffer from them at some point in their lives.
Hemorrhoids, swollen or inflamed veins in the rectal and anal area, can present with a variety of symptoms depending on their type and severity. There are three main types: internal hemorrhoids, external hemorrhoids, and thrombosed hemorrhoids. Each type has characteristic signs and symptoms.
Common hemorrhoid symptoms
Symptoms common to all three types of hemorrhoids include:
- Rectal bleeding, usually bright red.
- Anal itching or irritation.
- Pain or discomfort around the anus.
- Swelling or lumps near the anal opening.
- Mucus discharge.
- Difficulty with hygiene and possible foul odor.
- Sensation of incomplete bowel evacuation or fullness.
Internal hemorrhoids
The specific symptoms of internal hemorrhoids include:
- Often painless, especially in early stages, because internal rectal tissue lacks pain-sensitive nerve endings.
- Bright red bleeding during bowel movements is common, noticeable on toilet paper, in the toilet bowl, or on stool.
- A feeling of incomplete evacuation or fullness.
- Prolapse (when hemorrhoids push through the anal opening)
- May cause discomfort or pain.
- May feel like lumps around the anus, sometimes pink or red.
- Can retract on their own or be manually pushed back.
- Itching and irritation around the anus due to mucus or stool residue.
- Possible mucus discharge.
Internal hemorrhoids are often graded by their degree of prolapse:
- Grade 1: No prolapse.
- Grade 2: Prolapse but retracts spontaneously.
- Grade 3: Prolapse requiring manual reduction.
- Grade 4: Prolapse that cannot be manually reduced and may cause significant pain.
External hemorrhoids
External hemorrhoids, located under the skin around the anus, have several common signs and symptoms:
- Itching or irritation around the anus (pruritus ani).
- Pain and discomfort, especially while sitting or with bowel movements.
- Swelling or palpable lumps near the anus.
- Hemorrhoidal bleeding, though usually less than that of internal hemorrhoids.
- Difficulty cleaning the area after defecation due to swelling or mucus.
External hemorrhoids can become visibly swollen, often bluish or purplish due to blood pooling.
Thrombosed hemorrhoids
Thrombosed hemorrhoids occur when blood clots develop inside a hemorrhoid (internal or external), and symptoms include:
- Sudden and severe pain near the anus.
- Swelling and hard lumps that feel tender or painful.
- Bluish or purplish discoloration around the lump.
- Inflammation and sometimes difficulty sitting.
This condition is often acute and can require medical treatment.
The main risk factors for hemorrhoids are lifestyle-related, but also include medical conditions and biological characteristics. Key risk factors are:
- Sex: Women are more prone to hemorrhoids.
- Age: Hemorrhoids are more common as people get older, especially over age 50, because the tissues that support the veins in the rectum and anus weaken and stretch over time.
- Constipation and straining: Chronic constipation and repeated straining during bowel movements place excessive pressure on rectal veins, increasing the risk.
- Diarrhea: Frequent diarrhea can also irritate and inflame the anal area, contributing to hemorrhoid formation.
- Pregnancy: The weight of the baby in the abdomen during pregnancy increases pressure on the rectal veins. Hormonal changes also relax the veins and muscles, making hemorrhoids more likely.
- Obesity: Excess body weight contributes to increased abdominal pressure and venous congestion in the pelvic region.
- Prolonged sitting or standing: Sitting for long periods, especially on the toilet, or standing for extended periods can promote blood pooling in the anal area, raising vein pressure.
- Sedentary lifestyle: Lack of exercise decreases circulation and gut motility, which can contribute to constipation and vascular issues
- Low-fiber diet: A diet lacking in fiber can lead to constipation and harder stools, which can cause straining.
- Heavy lifting: Frequently lifting heavy objects increases abdominal pressure, which may aggravate hemorrhoids.
- Family history: Genetics may play a role, as hemorrhoids can run in families.
- Autoimmune disease history: Autoimmune diseases like Hashimoto’s, celiac, rheumatoid arthritis, and others may cause gut symptoms that increase the risk of hemorrhoids.
- Other medical conditions: Liver disease, heart disease, and inflammatory bowel conditions such as Crohn’s disease or irritable bowel syndrome (IBS) may increase susceptibility.
In summary, hemorrhoids develop primarily due to increased pressure and straining in the lower rectum and anus, with risk enhanced by lifestyle, medical, and genetic factors.
.webp)
Emerging research shows that people with hemorrhoids may be more likely to develop hypothyroidism, especially when caused by Hashimoto’s thyroiditis, and vice versa. We don’t have statistics that define a percentage of people with hypothyroidism who also have hemorrhoids. It’s also well established that people with hemorrhoids have a higher risk of developing hypothyroidism.
The role of constipation
Studies consistently show an association between these conditions due to shared risk factors, mainly chronic constipation.
Thyroid hormone acts as a kind of “metabolic accelerator” for your gut.
- In hypothyroidism, the entire gastrointestinal tract slows down.
- Peristalsis is reduced, so waste moves more slowly.
- The colon absorbs more water from the stool, making it harder and drier
- Stool sits longer in the colon and becomes hard and dry—harder to pass.
- Chronic hard stools mean more straining, pressure, and trauma to the veins around the rectum—causing or worsening hemorrhoids.
Even subclinical hypothyroidism (where blood tests are only mildly abnormal, yet symptoms are present) can cause noticeable digestive slowing and constipation.
For these reasons, constipation is one of the most consistent symptoms of hypothyroidism.
The gut-brain connection
The gut has a nervous system—a network called the enteric nervous system. Hypothyroidism (especially when caused by autoimmune Hashimoto’s) can affect the gut by disrupting this system, further compounding digestion issues. Poor gut health and inflammation (sometimes described as “leaky gut”) are also common in Hashimoto’s, and the resulting problems can both worsen constipation and make hemorrhoids more likely.
Other shared risk factors and triggers
Many risk factors overlap or interact:
- Obesity: Raises risk for both hemorrhoids and hypothyroidism. Obesity can also be a symptom of hypothyroidism.
- Physical inactivity: Leads to decreased gut motility and blood stasis, triggering both conditions.
- Poor diet: Low fiber increases constipation; inadequate nutrients can harm thyroid and gut health.
- Pregnancy and hormonal imbalances: Hormone changes affect both venous pressure around the anus and thyroid function.
Autoimmune and systemic effects
Hashimoto’s thyroiditis isn’t just about low thyroid hormones—it’s also an autoimmune disease with effects on multiple organs. Immune system dysregulation can cause inflammation and altered gut function, increasing the risk of hemorrhoids as well.
What does the research say?
One major nationwide study from Taiwan using health insurance data found patients with hemorrhoids were twice as likely to be later diagnosed with Hashimoto’s thyroiditis, compared to people who did not have hemorrhoids. Though the connection is not a direct “cause and effect,” it’s a statistically significant association:
- Incidence of Hashimoto’s in hemorrhoid patients: 5.37 per 1,000 person-years
- Incidence in controls: 2.46 per 1,000 person-years
- Relative risk: 2.06 times higher in the hemorrhoid group
This doesn’t mean everyone with hemorrhoids will get hypothyroidism, or vice versa. It does justify greater awareness and early problem-solving—especially when symptoms overlap.
As women approach and move through perimenopause and menopause, they experience significant changes in hormone levels, specifically, a decline in estrogen and progesterone. This transition isn’t just about hot flashes, night sweats, or mood swings—it has direct effects on many systems in the body, including digestive health and the integrity of vascular tissue. Research increasingly reveals a clear link between these hormonal changes and a rising incidence of hemorrhoids in women during midlife and beyond.
There are a variety of reasons why the risk of hemorrhoids goes up during the mid-life hormonal transition.
- Estrogen decline weakens tissues: Estrogen helps maintain the strength and elasticity of blood vessels, the connective tissue supporting rectal veins, and the pelvic floor muscles. Lower estrogen leads to weaker connective tissues and blood vessel walls, making them more vulnerable to stretching and swelling—prime conditions for hemorrhoids to develop or worsen.
- Reduced collagen and elastin: Along with estrogen, levels of collagen and elastin (proteins critical for tissue integrity) fall, which further weakens structural support in the anal and rectal areas.
- Slower digestion and constipation: Hormonal shifts can result in gastrointestinal sluggishness, slowing the movement of stool through the colon. The outcome? Constipation becomes more common, and the straining associated with passing hard stools dramatically increases pressure on rectal veins—one of the primary triggers for hemorrhoid development.
- Pelvic floor muscle changes: Hormonal and age-related weakening of the pelvic floor muscles reduces support for the veins around the anus. This weakens the natural mechanisms that prevent veins from bulging and forming hemorrhoids.
- Weight and activity changes: Menopause is often accompanied by weight gain and lower physical activity levels, both of which further contribute to constipation and increased abdominal pressure—two potent hemorrhoid risk factors.
Diagnosing hemorrhoids involves a combination of a detailed medical history, a physical exam, and, if necessary, specialized procedures to visualize the inside of the anus and rectum.
Medical history review
The healthcare provider starts by asking about:
- Symptoms such as bleeding, pain, itching, or lumps
- Bowel habits, including frequency, stool consistency, and straining
- Diet, use of laxatives or enemas
- Any personal or family history of digestive diseases, including colorectal cancer
- Other health conditions that may impact bowel function or venous health
This comprehensive history helps guide the physical exam and determines if further testing is needed.
Physical exam
- External inspection: The area around the anus is visually examined for external hemorrhoids, swelling, lumps, skin tags, signs of irritation, or blood.
- Digital rectal exam (DRE): The doctor inserts a gloved, lubricated finger into the rectum to feel for internal hemorrhoids, lumps, tenderness, or irregularities. This exam helps to check the tone of the anal muscles and detect any unusual masses.
Diagnostic procedures for internal hemorrhoids
If internal hemorrhoids are suspected or if symptoms suggest other conditions, the following procedures may be performed:
- Anoscopy: A small, hollow, lighted tube called an anoscope is inserted into the anus to directly view the lining of the anal canal and lower rectum. This allows the doctor to look for internal hemorrhoids, bleeding sources, or other abnormalities. It is usually done without anesthesia during an office visit.
- Proctoscopy/rigid sigmoidoscopy: These use longer tubes to examine the lower rectum and part of the colon. This exam provides more extensive visualization beyond the anus and anus canal.
- Flexible sigmoidoscopy: A flexible, lighted tube is used to inspect the rectum and sigmoid colon in more detail. Patients prepare with bowel cleansing beforehand.
- Colonoscopy: In cases of significant or unexplained rectal bleeding or to rule out other diseases like colon cancer, a colonoscopy may be done. It allows inspection of the entire colon using a flexible camera. This procedure requires sedation and bowel preparation.
Imaging tests
In rare cases where hemorrhoids are complicated or other concerns arise, imaging studies such as MRI or ultrasound may help evaluate surrounding blood vessels or detect other abnormalities.
If you are hypothyroid or going through perimenopause/menopause, it’s essential to treat any hormonal deficiencies and optimize your hormonal function. Treating hypothyroidism, perimenopause, or menopause doesn’t eliminate hemorrhoids directly, but it can significantly reduce their incidence and severity.
For your thyroid, that involves:
- Regular testing, including TSH, free T4, free T3, and thyroid peroxidase (TPO) antibodies
- Thyroid hormone replacement treatment: With medications to restore your thyroid hormone levels.
- Address nutrient deficiencies: Ensure adequate selenium, zinc, vitamin D, and B vitamins.
- Review your gut health: Probiotics, fermented foods, and addressing “leaky gut” can improve both thyroid symptoms and bowel function.
For women in perimenopause or menopause, some additional approaches can help, including:
- Hormone replacement therapy (HRT): HRT can help improve tissue and vascular integrity by replacing declining estrogen, potentially slowing the weakening of connective tissues that predispose women to hemorrhoids. Hormone replacement therapy is not prescribed specifically to treat hemorrhoids, but it may help support hemorrhoid treatment.
- Pelvic floor therapy: Targeted exercises or therapy for pelvic floor dysfunction can restore some of the muscle support lost with aging and hormonal changes, supporting rectal blood vessels and lowering hemorrhoid risk.
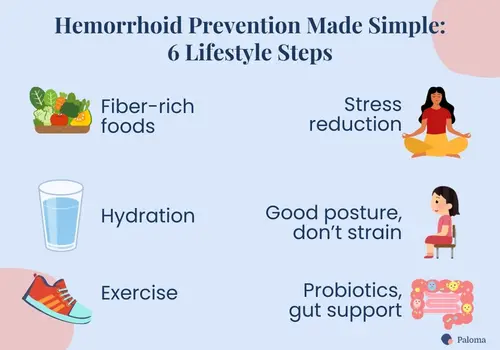
The good news is that there are simple lifestyle and nutritional changes you can make that can provide significant relief from hemorrhoids and help prevent future flare-ups. Whether you’re dealing with occasional irritation or more persistent symptoms, here are some practical and effective ways to manage hemorrhoids at home and through healthy habits.
Increase your fiber intake
One of the most important steps to ease hemorrhoid symptoms is to prevent constipation and make bowel movements easier. Eating a diet rich in fiber softens stools and helps them pass more smoothly, reducing strain on the veins around the anus.
- Aim to include plenty of fruits, vegetables, whole grains, and legumes.
- Gradually increase fiber to avoid gas or bloating.
- Fiber supplements like psyllium husk can also be helpful if dietary changes alone are not sufficient.
(You may even want to consider jumping on a current trend, “fibermaxxing,” to up your fiber intake!)
Stay hydrated
Drinking enough water is just as important as eating fiber to keep stools soft. Aim for 6 to 8 glasses of water per day to maintain good hydration, which supports regular and comfortable bowel movements.
Supplement with probiotics
Probiotics are beneficial microorganisms that naturally inhabit the gut and contribute to a balanced and healthy microbiome. Supplementing with probiotics can help:
- Restore gut flora balance: Antibiotics, poor diet, and stress can disrupt the natural gut microbiome, leading to digestive issues such as constipation or diarrhea.
- Improve bowel regularity: By promoting healthy digestion and stool consistency, probiotics can reduce constipation and the associated straining that worsens hemorrhoid symptoms.
- Support immune function: A healthy gut microbiome supports the immune system, which may help reduce inflammation and promote healing of irritated hemorrhoidal tissue.
Common probiotic strains used for digestive health include Lactobacillus and Bifidobacterium species. Probiotics can be found in supplements or fermented foods such as yogurt, kefir, sauerkraut, and kimchi.
Avoid excessive intake of ultra-processed foods and sugar
Diets high in processed foods and sugar can disrupt gut bacteria balance and exacerbate constipation. Whole foods rich in fiber, vitamins, and minerals support gut health and regular bowel function.
Get regular exercise
Physical activity is essential for maintaining overall health and benefits digestive function in several ways:
- Stimulates bowel motility: Exercise encourages the muscles in the intestines to contract, facilitating the movement of stool through the digestive tract and preventing constipation.
- Enhances circulation: Improved blood flow helps maintain healthy veins and prevents blood pooling in the pelvic and rectal areas, reducing the risk of hemorrhoids.
- Supports weight management: Maintaining a healthy weight decreases abdominal pressure, lowering the strain on the veins around the anus.
Beyond planned exercise, staying active throughout the day—standing up frequently, stretching, and walking—contributes to better digestion and reduces venous pressure in the lower body.
Reduce your stress
Chronic stress negatively impacts gut motility by disrupting the brain-gut axis. Stress can slow digestion, cause constipation, and worsen symptoms of hemorrhoids. Stress management techniques such as mindfulness, meditation, deep breathing exercises, or gentle exercise can help manage stress levels.
Maintain good posture
Sitting for long periods increases pressure on the rectal veins, which can contribute to hemorrhoid development or worsen existing symptoms. Practice good ergonomic habits at work, use supportive seating, take regular breaks to stand or walk, and avoid prolonged sitting on the toilet, which can increase strain on the anus.
Don’t delay bowel movements
Responding promptly when you feel the urge to go helps prevent constipation from developing. Holding in stools can cause them to become dry and hard, making them more difficult to pass and increasing the risk of straining.
Consider natural supplements and topical remedies
Several natural products have been studied for their potential benefits in managing hemorrhoid symptoms. For example, fig leaf extract (Ficus carica) has shown strong anti-inflammatory and wound-healing effects, with clinical trials showing healing rates exceeding 85%—outperforming some commercial topical medications. Cissus quadrangularis is another supplement with anti-inflammatory benefits. Similarly, eggplant extract (Solanum melongena) has been shown to reduce inflammation in hemorrhoidal tissue. Flavonoid mixtures that include diosmin, hesperidin, and rutin help minimize bleeding and swelling, and professional guidelines support their use. Finally, while not directly treating hemorrhoids, senna (Senna alexandrina) is a natural stimulant laxative that can ease constipation and reduce straining, indirectly alleviating hemorrhoid symptoms.
Try warm soaks and topical treatments
Taking warm sitz baths (soaking the anal area with warm water for 10–15 minutes) several times a day can relieve pain, reduce swelling, and promote healing. Over-the-counter creams, ointments, or wipes containing soothing ingredients like witch hazel or hydrocortisone may help ease itching and discomfort.
Minimize straining and prolonged sitting
Straining during bowel movements increases pressure on hemorrhoidal veins, worsening symptoms. To reduce straining:
- Avoid pushing hard during bowel movements.
- Consider using a footstool (i.e., a “squatty potty”) to elevate your feet while sitting on the toilet, which can make elimination easier.
- Try not to sit on the toilet for extended periods, as prolonged sitting increases venous pressure around the anus.
Use stool softeners when needed
If you are taking medications such as thyroid hormone replacement or experiencing constipating conditions like menopause-related hormonal changes, stool softeners can be valuable. They help prevent hard stools and reduce the need for straining.
When lifestyle changes are not enough, medical treatments can help relieve symptoms, shrink hemorrhoids, and prevent complications. The type of treatment depends on the severity of the hemorrhoids and symptoms.
Rubber band ligation
Rubber band ligation is a common outpatient procedure that involves placing a small rubber band around the base of an internal hemorrhoid to cut off its blood supply. The hemorrhoid shrinks and falls off within a week. It is effective for moderate hemorrhoids causing bleeding or prolapse.
Sclerotherapy
In sclerotherapy – a minimally invasive treatment – a chemical solution is injected into hemorrhoidal tissue to shrink it. It is often used for smaller internal hemorrhoids and offers quick relief with minimal discomfort.
Infrared, laser, or bipolar coagulation
Coagulation techniques use heat or light energy to coagulate hemorrhoid tissue, causing it to shrink. They are usually reserved for early-stage internal hemorrhoids and performed in a doctor’s office.
Hemorrhoidectomy
For severe or persistent hemorrhoids, especially large or thrombosed external hemorrhoids, or those causing significant pain or bleeding, surgical removal may be necessary. Hemorrhoidectomy is the most effective treatment for advanced cases but involves a longer recovery.
Stapled hemorrhoidopexy
Stapled hemorrhoidopexy is a surgical procedure that cuts off blood flow to hemorrhoids and lifts prolapsed tissue back into place. It usually results in less pain and a faster recovery than traditional hemorrhoidectomy, but it is suitable for select cases.
Medications
Various medications may help deal with hemorrhoids. They include:
- Topical creams and suppositories: Containing hydrocortisone or other anti-inflammatory agents to reduce swelling and discomfort.
- Pain relievers: Over-the-counter options like acetaminophen or ibuprofen can help ease pain.
Hemorrhoid symptoms can overlap with other medical conditions, such as anal fissures or colorectal diseases, so proper medical evaluation is essential to ensure accurate diagnosis and treatment.
It’s critical to consult a practitioner if you notice any of the following signs or symptoms:
- Persistent bleeding or pain lasting more than a week.
- Large amounts of rectal bleeding.
- Painful lumps that do not improve.
- Persistent abdominal pain or unexplained weight loss.
- Any changes in bowel habits or stool color.
- Symptoms that interfere significantly with your daily life.
Most hemorrhoids can be managed with simple lifestyle changes—more fiber, better hydration, and less straining. When symptoms are severe or don’t improve with home care, safe and effective medical treatments are available to bring relief and restore comfort. If you notice significant bleeding, ongoing pain, or persistent symptoms, it’s important to see a healthcare provider for personalized care.
What’s often overlooked is that hemorrhoids don’t always exist in isolation. Research shows surprising links between hypothyroidism—particularly Hashimoto’s—and hemorrhoids. Add in the hormonal shifts of perimenopause and menopause, and the risk climbs even higher. Constipation is the common thread here: both a sluggish thyroid and midlife hormone changes can slow digestion, increase straining, and put extra pressure on rectal veins. Poor gut health, nutrient deficiencies, and reduced activity only add fuel to the fire.
While thyroid disease and menopausal changes don’t directly cause hemorrhoids, understanding these overlapping risk factors gives you an important head start. If you or someone you know struggles with recurring hemorrhoids alongside symptoms of low thyroid or the hormonal changes of midlife, it may be time to consider hormone and thyroid testing.
That’s where Paloma Health comes in. As the first virtual clinic focused on hormonal health – including hypothyroidism and Hashimoto’s, perimenopause, and menopause, you can get everything you need to take control of your thyroid and hormonal health from home. With Paloma, you can:
- Test your thyroid at home with Paloma’s simple finger-prick thyroid test kit that delivers accurate, certified lab results.
- Meet via video visits with savvy healthcare professionals who specialize in hypothyroidism, Hashimoto’s, and midlife hormonal changes like perimenopause and menopause.
- Get a personalized care plan that integrates lifestyle, nutrition, and medication adjustments to support digestion, balance hormones, and improve overall comfort.
By improving thyroid function, balancing your hormones, and building healthier daily habits, you can not only reduce the risk of hemorrhoids but also boost your energy, comfort, and quality of life!
- Hemorrhoids are common, affecting up to half of people at some point in their lives.
- Constipation is the strongest shared link between hemorrhoids, hypothyroidism, and menopause.
- Hypothyroidism slows digestion, leading to hard stools and straining that increases the risk of hemorrhoids and makes existing hemorrhoids worse.
- Declining estrogen during menopause weakens tissues and blood vessels, raising the risk.
- Lifestyle steps—fiber, hydration, exercise, and stress reduction—are the foundations of prevention and relief from hemorrhoids.
- Addressing thyroid and hormonal health with testing and treatment can lower the risk of developing hemorrhoids and reduce the frequency and severity of the condition.

.webp)












