In this article
If you have Hashimoto’s thyroiditis or hypothyroidism, you may have heard — or personally experienced — a frustrating reality: you don’t feel fully well even after diagnosis and treatment. You take your medication, your lab results show up as “normal,” yet your fatigue, brain fog, weight challenges, and mood changes persist.
This experience is not rare — and it’s not “all in your head.” A growing body of research confirms that thyroid patient dissatisfaction is widespread and rooted in real biological, clinical, and communication gaps.
At Paloma Health, we hear these concerns every day. The good news? Thyroid care is evolving. In this article, we’ll explore what the research reveals about dissatisfaction—and how patient-centered care models like Paloma’s are helping thyroid patients finally feel better.
A quiet, largely unrecognized epidemic is unfolding in thyroid care. It’s not missed diagnoses, but rather patients who are diagnosed, treated, and remain unwell. On paper, these patients are “managed.” In reality, many are struggling. They take their medication faithfully. Their lab results fall within the reference ranges. Yet the fatigue lingers. Brain fog clouds their thinking. Weight refuses to budge. Mood shifts strain relationships and confidence. And perhaps most distressing of all, they often feel totally alone in that experience.
Large international surveys reveal a strikingly consistent pattern: dissatisfaction among people with hypothyroidism is common, widespread, and deeply tied to daily quality of life. A 2022 global survey of 3,915 patients across 68 countries, published in PubMed, found that dissatisfaction was strongly associated with two major factors — lack of trust in healthcare providers and the persistent burden of symptoms. In other words, it wasn’t simply about medication choice. It was about how patients felt, both physically and relationally. When symptoms continued, and communication faltered, dissatisfaction grew.
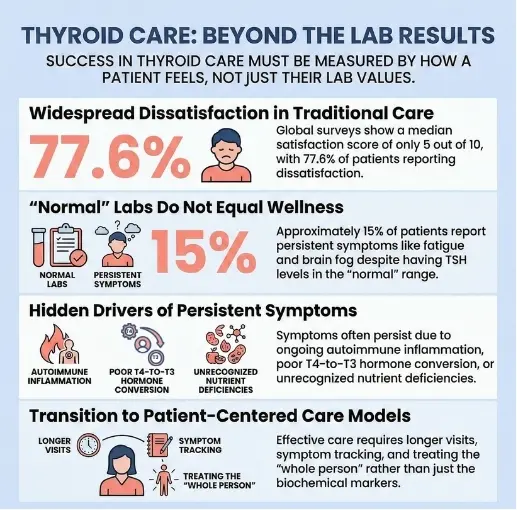
Another large survey of more than 12,000 hypothyroid patients, reported through the Mayo Clinic platform, found a median treatment satisfaction score of just 5 out of 10. That’s not a small dip in contentment — it’s a glaring signal that many patients feel only halfway helped. Persistent symptoms were common despite treatment, underscoring a critical truth: biochemical control does not always translate into lived wellness.

The numbers become even more sobering when looking at data from the British Thyroid Foundation, which found that 77.6% of respondents reported dissatisfaction with treatment or quality of life. When more than three-quarters of patients report feeling dissatisfied, it is no longer an isolated issue. It is systemic. It is cultural. It is a gap between what medicine measures and what patients experience. A British Thyroid Foundation survey found that 77.6% of patients were dissatisfied with treatment or quality of life.
Why does this matter so much? Hypothyroidism is not a rare condition. Millions of people worldwide live with it, many due to Hashimoto’s thyroiditis, an autoimmune disease that often requires lifelong management. When such a large patient population reports feeling unheard, unwell, or unsupported, the ripple effects extend far beyond individual frustration. Productivity declines. Mental health suffers. Relationships strain. Confidence erodes. Over time, chronic symptoms can reshape how someone sees themselves and their future.
What makes this epidemic “hidden” is that traditional metrics of success — TSH levels in range, prescriptions filled, follow-up labs completed — suggest that the system is working. But patient-reported data tell a different story. Studies, anecdotal reports, and patient forums reveal a disconnect between numbers and narrative. Between laboratory normalization and real-world vitality. Between treatment and true well-being.
Perhaps most importantly, the research points to trust as a central driver of satisfaction. Patients who feel listened to, respected, and engaged in shared decision-making report better experiences — even when their treatment plan is similar. This underscores a profound truth: thyroid care is not only biochemical; it is relational. Healing is not just about hormone levels. It is about partnership.
The growing body of international data is shining light on what many thyroid patients have known for years: feeling unwell despite treatment is common, and dissatisfaction is not imagined. It is measurable. It is validated. And acknowledging it is the first step toward meaningful change.
One of the most common — and most discouraging — experiences in hypothyroidism is being told your TSH is “normal” while you still feel anything but normal. You may leave your appointment with reassurance that your labs look good, yet continue to struggle with exhaustion, mental fogginess, mood changes, or stubborn weight gain. Over time, this disconnect between numbers and lived experience can feel confusing and invalidating.
Importantly, this situation is not rare. Research summarized by the American Thyroid Association indicates that approximately 15% of patients report ongoing symptoms despite having TSH levels within the reference range. In other words, a significant group of people treated for hypothyroidism continues to feel unwell even when their lab results suggest their condition is adequately managed.
Part of the issue is that TSH — thyroid-stimulating hormone — is a regulatory signal from the brain to the thyroid. While it is an important marker, it does not directly measure how thyroid hormone is functioning inside your cells and tissues. Two people can have identical TSH values but feel very different. Lab ranges are also broad, and “normal” does not necessarily mean “optimal” for every individual. Thyroid hormone activity is influenced by conversion processes, immune activity, inflammation, stress levels, nutrient status, and other hormonal systems — none of which are fully captured by a single blood test.
Common persistent symptoms
Many patients with normalized labs report symptoms such as:
- Fatigue and low energy – A deep, persistent tiredness that doesn’t improve with rest and can make everyday tasks feel overwhelming.
- Brain fog and memory issues – Difficulty concentrating, slower thinking, forgetfulness, or feeling mentally “cloudy.”
- Weight gain or resistance to weight loss – Especially when diet and exercise efforts don’t seem to produce expected results.
- Depression or anxiety – Mood shifts, low motivation, irritability, or heightened worry that may not have been present before thyroid dysfunction.
- Hair loss – Thinning hair, brittle strands, or changes in texture.
- Cold intolerance – Feeling unusually cold compared to others, particularly in the hands and feet.
These symptoms are real — and they are not simply the result of stress or imagination. Research increasingly shows that persistent symptoms can have multiple, overlapping causes. Ongoing autoimmune activity in Hashimoto’s, challenges converting T4 to active T3 hormone, nutrient deficiencies (such as iron or vitamin D), perimenopausal hormonal shifts, sleep disturbances, metabolic factors, and mental health conditions can all contribute. When care focuses solely on bringing TSH into range without exploring these additional layers, important drivers of symptoms may be missed.
Understanding that “normal labs” do not always equal “feeling well” is an important first step. It opens the door to a broader, more individualized approach—one that considers the whole person, not just the numbers on a page.
Living with Hashimoto’s or hypothyroidism can feel confusing and discouraging when your lab results look “normal,” but you still don’t feel well. Many people continue to struggle with fatigue, brain fog, mood changes, and other symptoms even after starting treatment. Research now shows this is not only common, but often has multiple overlapping causes — including autoimmune activity, thyroid hormone processing, other health conditions, and emotional factors.
Autoimmune activity in Hashimoto’s
Hashimoto’s is first and foremost an autoimmune disease, not just a simple hormone deficiency. In Hashimoto’s, the immune system mistakenly targets the thyroid gland, creating ongoing inflammation and antibody production that can affect how you feel day to day. Even when thyroid hormone levels are brought into the normal range with medication, that immune activity may still be simmering in the background.
Studies show that people with Hashimoto’s can have a reduced quality of life compared to those without the disease, even when their thyroid hormone levels are normalized. Hashimoto’s patients often report more fatigue, emotional distress, and physical limitations than would be expected based on labs alone.
What this means in real life:
- Ongoing autoimmune activity may contribute to fatigue that doesn’t fully improve with medication.
- Inflammation and immune dysregulation may play a role in mood changes, such as anxiety or low mood.
- Some patients notice cognitive symptoms such as brain fog, slower thinking, or trouble focusing, even when their TSH is normal.
In other words, “normal labs” don’t always mean the autoimmune process has quieted down — and that lingering immune activity can still influence how you feel.
Thyroid hormone conversion challenges
Many people with hypothyroidism are treated with levothyroxine (T4), a synthetic form of the main hormone produced by the thyroid. T4 itself is mostly a storage hormone. To have its full effect, your body must convert T4 into T3, the active hormone that actually enters cells and helps regulate energy, mood, metabolism, and brain function.
Some patients may not convert T4 to T3 efficiently due to genetics, illness, medications, nutrient deficiencies, or other factors. When that conversion is less effective, you can end up with:
- Thyroid labs that look “in range” on paper
- But tissue-level low T3, which may contribute to persistent symptoms like fatigue, weight changes, or brain fog
Research and clinical experience have led to ongoing discussions about combination therapy (T4 + T3) for people who remain symptomatic on levothyroxine alone. While this approach isn’t right for everyone, it reflects a growing recognition that thyroid hormone conversion is complex — and that some patients may need more individualized treatment strategies.
Overlapping health conditions
Thyroid health rarely exists in isolation. Many conditions that commonly occur alongside hypothyroidism can mimic or worsen thyroid-like symptoms. If these aren’t recognized and addressed, patients may remain symptomatic even when their thyroid is treated. Common overlapping factors include:
- Iron deficiency: Low iron or ferritin can cause fatigue, shortness of breath, hair loss, and reduced exercise tolerance, and is especially common in people assigned female at birth.[frontiersin]
- Vitamin D deficiency: Low vitamin D levels have been linked to autoimmune thyroid disorders and may be associated with disease severity and progression.functionhealth+1
- Perimenopause and menopause: Shifting estrogen and progesterone levels can cause hot flashes, mood changes, sleep problems, and brain fog, which often overlap with hypothyroid symptoms.
- Insulin resistance and blood sugar issues: Insulin resistance is more common in people with thyroid dysfunction and can contribute to fatigue, abdominal weight gain, and increased cardiovascular risk.[frontiersin]
- Depression and anxiety: Mood disorders are more prevalent in people with thyroid conditions and can independently cause low energy, poor concentration, sleep changes, and reduced quality of life.pmc.ncbi.nlm.nih+1
If care focuses only on TSH and thyroid hormone levels without checking for these related issues, it’s easy to miss important pieces of the puzzle. A more complete evaluation that includes nutrients, metabolic health, hormonal transitions, and mental health can be key to feeling better.

Psychological and expectation factors
It’s also important to acknowledge the role of expectations and emotional well-being in how satisfied you feel with their thyroid care. Research suggests that persistent symptoms on levothyroxine are often multifactorial — involving not only biology, but also related conditions, stress, past health experiences, and what you hope treatment will achieve.
This does not mean symptoms are “all in your head.” Instead, it highlights that:
- Feeling unheard, dismissed, or rushed during appointments can increase frustration and dissatisfaction.
- Chronic illness can understandably affect mood, confidence, and hope over time.
- When care addresses both physical and emotional needs — through clear communication, shared decision-making, and supportive relationships — patients often feel more empowered and satisfied, even as treatment is fine-tuned.
Whole-person care that validates the reality of symptoms, explores realistic treatment goals, and offers ongoing support can make a meaningful difference in both quality of life and how patients experience their thyroid journey.
Levothyroxine remains the standard treatment for hypothyroidism— and it is essential. However, research shows that biochemical normalization alone does not guarantee symptom relief.
A pooled analysis of randomized trials found no significant difference in treatment satisfaction between levothyroxine and placebo in some groups.
This tells us that:
- Thyroid care must go beyond lab values
- Symptom relief requires individualized care
- Patient experience matters as much as lab results
Quality-of-life research using validated tools like the ThyPRO questionnaire reveals that many people living with Hashimoto’s thyroiditis experience a wide range of daily challenges — even when their thyroid hormone levels appear perfectly normal on lab tests.
Commonly reported issues include persistent fatigue, emotional distress or mood swings, trouble with concentration and memory, and limitations in social or work activities. These symptoms can make it difficult to maintain energy, motivation, and emotional balance, creating an invisible burden that often goes unrecognized by others.
This growing body of research underscores an important truth: autoimmune thyroid disease affects far more than just the thyroid gland. It impacts the whole person — their mind, emotions, and sense of well-being. Understanding this broader impact is key to providing care that addresses not only hormone balance but also overall quality of life.
.webp)
Research shows trust in healthcare providers is a stronger predictor of satisfaction than medication choice.
Patients frequently report:
- Feeling rushed during visits
- Symptoms being dismissed
- Overreliance on TSH alone
- Lack of shared decision-making
When patients feel unheard, dissatisfaction grows — even if treatment is technically correct.
In many conventional healthcare settings, doctors are pressed for time and resources, leading to visits that are often short and fragmented. Appointments typically last around 10 minutes, leaving little room for in-depth conversations, lifestyle guidance, or emotional support. Follow-up appointments may be weeks or even months apart, making it hard for patients to get consistent care or feel truly heard.
Most conventional visits also focus heavily on lab numbers — checking whether your thyroid levels fall within the “normal” range — rather than exploring how you actually feel and whether your levels are optimal. For patients with Hashimoto’s or hypothyroidism, this approach is often very frustrating. These conditions are complex, chronic, and deeply individual, often changing over time and influenced by many factors such as stress, gut health, nutrition, immune balance, and lifestyle.
That’s because thyroid health isn’t confined to one organ. It’s intimately connected to nearly every system in the body. When the thyroid slows down, it can affect:
- Metabolism, leading to fatigue, weight changes, and temperature sensitivity
- Mental and emotional health, contributing to anxiety, low mood, or brain fog
- Reproductive hormones, which can disrupt menstrual cycles and fertility
- Cardiovascular function, influencing cholesterol levels and heart rate
- Immune function often creates a cycle of inflammation and flare-ups
When care is fragmented — spread across multiple specialists with little coordination — you can easily end up feeling unsupported, confused, and left to manage symptoms on your own. A more holistic, team-based approach that looks beyond lab results and focuses on the whole person can make a world of difference for long-term thyroid health and well-being.
As dissatisfaction has become more widely recognized, new care models are emerging to address patient needs.
At Paloma Health, care is designed around the concerns patients report most often.
Treating the patient — not just the lab results
Because symptom burden drives dissatisfaction more than lab values, the best thyroid care emphasizes:
- Symptom tracking
- Quality-of-life assessments
- Personalized treatment adjustments
The goal is simple: help patients feel better, not just look better on paper.
Personalized treatment approaches

Since levothyroxine alone does not resolve symptoms for everyone, individualized care may include:
- Careful dose optimization
- Evaluation for T4-to-T3 conversion issues
- Addition of T3 therapy when necessary
- Consideration of combination therapy when appropriate
- Screening for nutrient deficiencies
New clinical trials now prioritize patient-reported outcomes when evaluating combination therapy.
This reflects a growing recognition that patient experience matters.
Addressing autoimmune and whole-body health
Hashimoto’s affects more than thyroid hormone levels. Comprehensive care may include:
- Nutritional evaluation
- Gut health considerations
- Stress and sleep support
- Screening for related autoimmune conditions
Addressing root contributors can improve quality of life.
Longer visits and better communication
Because trust strongly predicts satisfaction, patient-centered medical practices emphasize:
- Extended consultations
- Collaborative decision-making
- Education about lab results and symptoms
When patients feel heard and informed, satisfaction improves.
Integrated hormonal and metabolic care
Hypothyroidism often overlaps with:
- Perimenopause and menopause
- Weight management challenges
- Insulin resistance
Integrated care that accounts for these related conditions reduces frustration and improves outcomes.
.webp)
A major transformation is underway in the world of thyroid research and clinical care. For decades, success in treating thyroid disorders like Hashimoto’s hypothyroidism was primarily measured by laboratory values — for example, whether TSH, Free T4, and Free T3 levels fell within the “normal” reference ranges. While labs remain valuable, they don’t always tell the full story of how someone actually feels.
That’s where patient-reported outcomes (PROs) come in. Researchers are increasingly using PROs as primary endpoints in clinical trials, shifting the focus from lab results to the lived experiences of real patients.⁸ This evolution represents a deeply needed change — one that recognizes that good thyroid health is not just about hormone balance but about quality of life.
PRO tools such as the ThyPRO questionnaire and others are designed to capture how thyroid disease affects everyday functioning. These tools gather data directly from patients, asking them to rate their experiences in areas such as:
- Energy and fatigue levels – How much stamina they have during daily tasks
- Cognitive function – Whether they struggle with memory, focus, or mental clarity
- Emotional well-being – Feelings of anxiety, mood changes, or emotional stability
- Daily functioning – How well symptoms allow them to participate in work, relationships, and hobbies
- Symptom burden – The frequency and intensity of issues such as weight changes, temperature sensitivity, hair loss, or muscle aches
By measuring these human aspects of thyroid disease, researchers gain a more complete picture of what “better” truly means for patients. For example, someone may have thyroid hormone levels that appear optimal on paper, yet still feel profoundly tired or mentally foggy. When PROs are included, those experiences are no longer dismissed as “normal”—they become meaningful data guiding research, treatment, and clinical decision-making.
This paradigm shift reflects a growing recognition that numbers don’t heal people — care does. By centering the patient voice, the future of thyroid care is moving toward a more personalized, compassionate, and outcome-focused model. This approach promises to reduce long-standing dissatisfaction among thyroid patients who have felt unheard or overlooked, ensuring that the true measure of success is not only balanced labs but restored energy, clarity, and well-being.
If you’ve been told your thyroid levels are “normal” but you still don’t feel like yourself, you are absolutely not alone. So many people living with Hashimoto’s or hypothyroidism share this same experience — the lab results look fine, but the symptoms linger. The fatigue, brain fog, mood changes, and frustration can start to wear you down. But here’s the good news: there are real, practical steps you can take to start feeling better and ensure your care truly fits you.
Be your own advocate
It’s okay to speak up when something doesn’t feel right. You know your body better than anyone else. If you’re still struggling with symptoms, let your provider know exactly how these issues are affecting your day-to-day life. Think of your voice as an essential part of your care team. And if your concerns aren’t being heard or addressed? You deserve a provider who does listen.
Track what you’re feeling
Keeping a simple symptom diary can make a big difference. Whether you jot things down in a notebook or use a health app that tracks symptoms like HashiTrack, try tracking patterns — your energy levels, sleep, mood, or other symptoms — for a few weeks. Over time, you might notice what makes things better or worse. This kind of insight helps any provider see your full picture, not just a single lab result.
Explain what daily life is like
When you talk about your symptoms, connect them to your everyday experiences. Instead of just saying, “I’m tired,” try describing how that tiredness impacts you: “By midafternoon, I can barely get through my day.” This kind of detail helps your care team understand how much your symptoms affect your quality of life — and can lead to more personalized adjustments to your treatment.
Ask about nutrient testing
Sometimes, nutrient levels play a hidden role in how you feel. If you haven’t already, ask your provider whether testing things like iron, vitamin B12, vitamin D, zinc, iodine, or selenium might be helpful. Subtle deficiencies can worsen fatigue or brain fog, even when thyroid levels look normal. Addressing those gaps can sometimes make a big difference in how your body responds to thyroid medication.
Find a supportive care team
Thyroid health is deeply personal — and it deserves more than a one-size-fits-all approach. Look for collaborative, patient-centered providers who take the time to understand your unique situation and who value your input. Practices like Paloma Health focus on thyroid care that’s more personalized, holistic, and convenient, with providers who look at the big picture — your lifestyle, your lab results, and how you actually feel day to day.
Explore comprehensive thyroid care
If your current care still leaves you feeling unheard, you might benefit from a comprehensive thyroid approach. This often means working with a team that goes beyond adjusting medication — exploring nutrition, stress, gut health, hormones, and immune balance as part of one connected picture. With the right support, many people find they can finally start feeling like themselves again.
Takeaway
If you’re still symptomatic, remember this: it’s not “in your head,” and you don’t have to settle for feeling unwell. By tracking your symptoms, asking questions, and finding a provider who truly listens — whether locally or through a thyroid-focused practice like Paloma Health — you can take meaningful steps toward better energy, sharper thinking, and feeling whole again.
Over the past few years, a steady stream of research has brought something important to light: many people with Hashimoto’s and hypothyroidism still don’t feel well, even when their thyroid levels look “normal.” Studies from 2022 to 2026 have consistently shown that this dissatisfaction is widespread — and it’s not caused by just one thing. It’s multifactorial, meaning there are several overlapping reasons why patients may continue to struggle despite receiving treatment.
For some, it’s the persistence of symptoms like fatigue, brain fog, hair loss, or weight changes. For others, it’s the ongoing burden of autoimmune activity or the emotional impact of feeling unwell for so long. Add to that common gaps in communication and the time constraints of traditional healthcare — where visits often last 10 or 15 minutes — and it becomes easier to understand why many people leave appointments feeling unseen or unheard.
When we begin to see these patterns not as isolated complaints but as evidence of a widespread care gap, the path forward becomes clearer.
But there’s a shift happening—and it gives us hope.
Thyroid care is evolving. In recent years, researchers and clinicians alike have begun looking beyond lab results to understand how patients truly feel. This is where patient-reported outcomes (PROs) come in — tools that measure aspects like energy, mood, cognitive function, and quality of life directly from the patient’s perspective. The growing use of PROs in thyroid research marks an important change in how “success” is defined: it’s no longer just about bringing TSH into range, but about helping people feel well, function better, and live more vibrant lives.
At Paloma Health, we’re proud to be part of this evolution. Our care model is built on the belief that thyroid care should be as individual as you are. That means focusing not only on lab values but on the whole picture — convenient lab testing, your symptoms, goals, lifestyle, preferences, and lived experiences. Paloma’s team of thyroid-focused providers, dietitians, and health coaches works together to deliver care that’s more personal, more convenient, and more connected to your real-world experience.
This patient-centered approach reflects what research has been telling us all along: that when care includes partnership, communication, and a deeper understanding of each person’s story, outcomes improve—and so does quality of life.
For the millions of people living with thyroid disease, this new era of care offers something that’s been missing for far too long: validation, collaboration, and a clear path toward feeling genuinely better.
If you’re still feeling unwell despite “normal” labs, you’re not alone — and it doesn’t mean you’re imagining things. It often means there’s more to explore: immune activity, hormone conversion, nutrient status, overlapping conditions, and the emotional weight of living with a chronic illness. Understanding these layers is a powerful first step toward more personalized, compassionate, and effective thyroid care. Thyroid health isn’t just about balancing hormones — it’s about restoring energy, clarity, and confidence in your everyday life. And that’s exactly what Paloma is here to help you do!
Why do some hypothyroid patients still feel unwell even when their lab results are normal?
Thyroid symptoms can stem from ongoing autoimmune activity, hormone conversion issues, nutrient deficiencies, or overlapping health conditions — not just TSH levels alone.
Is it common to feel dissatisfied with thyroid treatment?
Yes. Large international surveys show that many patients report persistent symptoms and only moderate satisfaction with their care.
What exactly is Hashimoto’s thyroiditis?
Hashimoto’s is an autoimmune disease in which the immune system attacks the thyroid gland, often leading to hypothyroidism over time.
What symptoms most commonly persist despite treatment?
Fatigue, brain fog, difficulty losing weight, depression or anxiety, hair loss, and cold intolerance are among the most frequently reported ongoing symptoms.
What does it mean to have trouble converting T4 to T3?
Most thyroid medications contain T4, which must be converted into the active form, T3. Some people may not convert efficiently, which can contribute to lingering symptoms.
Can other health conditions mimic hypothyroid symptoms?
Yes. Iron deficiency, vitamin D deficiency, perimenopause, insulin resistance, and mood disorders can all cause symptoms that overlap with hypothyroidism.
What are patient-reported outcomes (PROs)?
Patient-reported outcomes are tools that measure how patients feel and function — including energy, mood, and cognitive clarity — rather than focusing only on lab numbers.
Does levothyroxine work for everyone?
Levothyroxine is the standard and essential treatment for hypothyroidism and works well for many people, but some patients may need individualized adjustments if symptoms persist.
Why does communication with healthcare providers matter so much?
Research shows that trust and feeling heard are strong predictors of satisfaction — sometimes even more important than the specific medication prescribed.
What can patients do if they’re still experiencing symptoms?
They can track symptoms, ask about comprehensive testing (including nutrients and hormone conversion), advocate for personalized care, and seek a provider who prioritizes quality of life alongside lab results.

.webp)
.webp)


.webp)
%20copy.webp)






